Prospective Transcriptomic Pathway Analysis of Human Lymphatic Vascular Insufficiency: Identification and Validation of a Circulating Biomarker
Important New Study out of Stanford University
http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0052021
StepUp-SpeakOut.Org BlogSpot
Hello and welcome to the StepUp-SpeakOut.Org Blog Spot.
We will be using this blog for fast updates on news and information in the field of Secondary Lymphedema as a result of Breast Cancer.
We will be posting articles and information on new research and treatments, legislative and insurance information, and other pertinent information, and invite your comments.
We will be using this blog for fast updates on news and information in the field of Secondary Lymphedema as a result of Breast Cancer.
We will be posting articles and information on new research and treatments, legislative and insurance information, and other pertinent information, and invite your comments.
Wednesday, December 19, 2012
Sunday, November 18, 2012
Tuesday, October 30, 2012
My Fat Arms--Writing about LE
From http://www.literarymama.com/columns/archives/2012/10/my-fat-arms.html
My Fat Arms
My Fat Arms
I would like to tell you about my fat arms, but it’s tricky. I’m afraid the tale will have you yawning with boredom, shifting in your chair wondering if there isn’t something else you’re supposed to be doing. You’ll get up to pour yourself a cup of coffee and never come back. So I have to think twice before I tell you that something has gone terribly wrong with an entire system of my body, a system that most people (and a disturbing number of medical professionals) have barely heard of and never studied.
There are reasons for this neglect. Though this system consists of a network of veins that thread all through our bodies—both directly below the skin and ever deeper and deeper into the very core of our being, servicing all the organs and body parts you ever memorized in sixth-grade science class—the fact remains that every tiny, pulsing micro-meter of it is practically invisible. And besides, it has an ugly name: the lymph system. Rhymes with nymph. Sounds like limp, or even lump.
You have felt your own lymph nodes, those pea-sized swellings in your armpit or groin when you have an infection somewhere in your body. Once the infection is over the nodes dwindle and disappear from your consciousness. That’s all most people know about the lymph system. That’s all they care to know. The lymph system does not inspire wonder.
But it should, because it has everything to do with staying well. The lymph network is the body’s dump truck. Those nearly invisible vessels that course from head to toe and everywhere in between are there to collect cell junk—bacteria, rogue cancer cells, even stray tattoo ink escaped from its intended place on the skin—and truck it to the nodes, where it’s rendered harmless or dispatched outright. They gather this junk by slurping up the body fluid that contains it, delivering it to the nodes, then returning it, cleaned and safe, into the circulatory system. Brilliant.
Which brings us right back to my fat arms. Are you still with me? Good, because we’re just getting to the heart of this matter: my lymph system has lost some of its capacity to slurp. Its pace has slowed, dulled by damage to the nodes in my chest and armpits from my cancer surgery and radiation. The body fluid accumulates, and my sluggish lymph system can’t collect it all. So it hangs out beneath the skin of my arms and chest, inflating them as though they were parts of a Macy’s Thanksgiving Day Parade balloon. Popeye arms, Mickey Mouse hands. Can I adjust to this perspective, alien and gawky, tethered just out of reach of the everyday world?
This ballooning is called lymphedema. I will learn ways to control it, but the damage is permanent. I’ll need to ignore the stares and questions, manage the pain of swollen body parts and develop new skills. For now, the cancer battle has been quelled, the treatment frenzy quieted, but the collateral damage involves disabilities I could never have imagined.
“You’d sure be surprised if I drove one home and parked it right in front of the house,” he says.
“I would.”
“What would all the neighbors say?” He’s smiling, relishing his private vision of the sidewalks lined with cheering neighbors gaping at his new-found might. He’s silent a moment, considering, and then, “Would I need a driver’s license?”
I nod again.
“But I don’t have one,” he says.
And he never will, so what is there to answer? “You could draw a garbage truck,” I try, “with you in the driver’s seat.” In Tony’s prolific artwork his vehicles all have personalities, sly or shy, fierce or furious. He doesn’t answer me, at least not with words. His eyes lose their light, though, and the conversation is clearly at an end.
So I wouldn’t tell you how it begins with five boring weeks of daily visits to a specially-trained therapist. She starts each session with an hour-long massage as intricate as the choreography for Swan Lake, minus the splendor and grace. The direction of each stroke matters, and so do the movements of her hands—cupping, smoothing, working delicate half-circles in precise patterns. Her touch is kitten-petting gentle, so as not to squish the tiny lymph vessels lying just beneath the skin, but rousing them instead to move the lymph fluid back toward the center of my body. And the pace is slow, with the slug-like rhythm of “Sunrise, Sunset” from The Fiddler on the Roof.
“Is this the little girl I carried?
Is this the little boy at play?
I don’t remember growing older…”
That slow.
After that she lotions each arm and wraps it in assorted medical-grade materials. Stockinette first, smoothed to the contours of my fat limb, and gauze to wrap my fingers, one by one. Then a sheet of thin, rolled foam that spirals up my arm from palm to armpit, followed by overlapping layers of short-stretch bandages, 16 feet long and medical-beige ugly. All of that helps the pumping of the lymph fluid, reducing the swelling even while I sleep. And as she does these things she teaches my clumsier hands to do them too, so I can spend a significant part of every day, for the rest of my life, doing the same at home.
Once the swelling is reduced the therapist fits me for compression garments—skin-tight sleeves, gloves and a vest—that I will wear every day. In every weather. For every occasion, whether casual or formal. Which is a concept I may never get my mind around.
I know where this discussion is headed and pretend I didn’t hear him while I think how to handle it.
He’s patient, but persistent. Within a few minutes he’s moved closer to me. “How about a pickup truck?” he says again, still not looking at me. When I don’t answer at once he adds the close to his remark: “I said.”
“You said that, yes.” I can think of no way to soften the blow. “There’s still the question of the driver’s license, though.”
He presses his lips into a flat line, and his brows furrow so deeply his dark eyes all but disappear.
Now that it’s me, though, I’m living this strange reality in which the crush injury of a blood pressure cuff will cause further damage to delicate lymph vessels, and injections or lab tests unbalance the careful choreography of lymph flow into and out of my limbs. Repetitive movements are off limits for me now, as is leaning my weight on my arms: no more crocheting or spinning wool, no more yoga downward dog.
“No, I guess not,” I tell him. “But you’d have to play golf.”
He ponders that a long moment. “A bike, then,” he says, and this time he’s peering directly into my face.
We’re bargaining, bringing lofty dreams into synch with our limiting realities—his and mine both. I want to give in and say yes, but his lack of critical judgment makes solo riding a nightmare. “Remember when that car rolled right over you?” Miraculously he wasn’t hurt when a neighbor backed out of his drive, right into Tony’s path. Boy and bike disappeared beneath the chassis—fortunately directly between the wheels. That was years ago but the memory is vivid. His eyes narrow, and he nods.
“A tandem,” I counter then. But as soon as the words leave my mouth I realize I’ve gone too far. When I lean my weight on those handlebars my arms will swell despite the hours a day I spend tending my traitorous lymph system.
“Okay,” he says, surrendering. “A tandem.” He flashes me a shy smile.
Suddenly nothing else matters—not the lymphedema, not even the autism. We’re going to make this work, Tony and me. We’ll figure out how to raise the handlebars and keep the weight off my arms. I’ll do the steering, but it will be Tony behind me, providing the pedal power, feeling the bracing whoosh of wind as we race along.
Maybe it’s not a garbage truck, but if the neighbors never line up along the sidewalk to cheer as we ride by, they’ll be missing a beautiful thing.
There are reasons for this neglect. Though this system consists of a network of veins that thread all through our bodies—both directly below the skin and ever deeper and deeper into the very core of our being, servicing all the organs and body parts you ever memorized in sixth-grade science class—the fact remains that every tiny, pulsing micro-meter of it is practically invisible. And besides, it has an ugly name: the lymph system. Rhymes with nymph. Sounds like limp, or even lump.
You have felt your own lymph nodes, those pea-sized swellings in your armpit or groin when you have an infection somewhere in your body. Once the infection is over the nodes dwindle and disappear from your consciousness. That’s all most people know about the lymph system. That’s all they care to know. The lymph system does not inspire wonder.
But it should, because it has everything to do with staying well. The lymph network is the body’s dump truck. Those nearly invisible vessels that course from head to toe and everywhere in between are there to collect cell junk—bacteria, rogue cancer cells, even stray tattoo ink escaped from its intended place on the skin—and truck it to the nodes, where it’s rendered harmless or dispatched outright. They gather this junk by slurping up the body fluid that contains it, delivering it to the nodes, then returning it, cleaned and safe, into the circulatory system. Brilliant.
Which brings us right back to my fat arms. Are you still with me? Good, because we’re just getting to the heart of this matter: my lymph system has lost some of its capacity to slurp. Its pace has slowed, dulled by damage to the nodes in my chest and armpits from my cancer surgery and radiation. The body fluid accumulates, and my sluggish lymph system can’t collect it all. So it hangs out beneath the skin of my arms and chest, inflating them as though they were parts of a Macy’s Thanksgiving Day Parade balloon. Popeye arms, Mickey Mouse hands. Can I adjust to this perspective, alien and gawky, tethered just out of reach of the everyday world?
This ballooning is called lymphedema. I will learn ways to control it, but the damage is permanent. I’ll need to ignore the stares and questions, manage the pain of swollen body parts and develop new skills. For now, the cancer battle has been quelled, the treatment frenzy quieted, but the collateral damage involves disabilities I could never have imagined.
* * *
“When I grow up,” says our autistic son Tony, heedless of the fact that he is already 30 years old, “I want to drive a garbage truck.” And why wouldn’t he, since it’s huge and powerful and makes an impressive roar and rumble, while it cleans up the environment and carries off everything that would otherwise sit rotting in the Arizona sun? Garbage truck drivers are environmental heroes, and they have the imposing equipment to back it up. With his assorted disabilities Tony is never going to hold a job, much less one that involves responsibility for a behemoth like that. It is hard to be both honest and encouraging about this dream of his, but I try. I nod and say, “That would be exciting, all right.”“You’d sure be surprised if I drove one home and parked it right in front of the house,” he says.
“I would.”
“What would all the neighbors say?” He’s smiling, relishing his private vision of the sidewalks lined with cheering neighbors gaping at his new-found might. He’s silent a moment, considering, and then, “Would I need a driver’s license?”
I nod again.
“But I don’t have one,” he says.
And he never will, so what is there to answer? “You could draw a garbage truck,” I try, “with you in the driver’s seat.” In Tony’s prolific artwork his vehicles all have personalities, sly or shy, fierce or furious. He doesn’t answer me, at least not with words. His eyes lose their light, though, and the conversation is clearly at an end.
* * *
If I tried to tell you what I have to do to move the swelling out of my arms and keep it that way—if for instance you came by one desert-hot afternoon, settled onto the couch with a welcome glass of cool water, ice clinking against the sides, and asked about my fat arms—when I started to answer, you would gaze down into the glass and swish the ice cubes in slow circles, and I would understand you were waiting for me to change the subject back to something more captivating.So I wouldn’t tell you how it begins with five boring weeks of daily visits to a specially-trained therapist. She starts each session with an hour-long massage as intricate as the choreography for Swan Lake, minus the splendor and grace. The direction of each stroke matters, and so do the movements of her hands—cupping, smoothing, working delicate half-circles in precise patterns. Her touch is kitten-petting gentle, so as not to squish the tiny lymph vessels lying just beneath the skin, but rousing them instead to move the lymph fluid back toward the center of my body. And the pace is slow, with the slug-like rhythm of “Sunrise, Sunset” from The Fiddler on the Roof.
“Is this the little girl I carried?
Is this the little boy at play?
I don’t remember growing older…”
That slow.
After that she lotions each arm and wraps it in assorted medical-grade materials. Stockinette first, smoothed to the contours of my fat limb, and gauze to wrap my fingers, one by one. Then a sheet of thin, rolled foam that spirals up my arm from palm to armpit, followed by overlapping layers of short-stretch bandages, 16 feet long and medical-beige ugly. All of that helps the pumping of the lymph fluid, reducing the swelling even while I sleep. And as she does these things she teaches my clumsier hands to do them too, so I can spend a significant part of every day, for the rest of my life, doing the same at home.
Once the swelling is reduced the therapist fits me for compression garments—skin-tight sleeves, gloves and a vest—that I will wear every day. In every weather. For every occasion, whether casual or formal. Which is a concept I may never get my mind around.
* * *
“Okay,” says Tony, apropos of nothing, as he sets the dinner plates around the table. “So, how about a pick-up truck?”I know where this discussion is headed and pretend I didn’t hear him while I think how to handle it.
He’s patient, but persistent. Within a few minutes he’s moved closer to me. “How about a pickup truck?” he says again, still not looking at me. When I don’t answer at once he adds the close to his remark: “I said.”
“You said that, yes.” I can think of no way to soften the blow. “There’s still the question of the driver’s license, though.”
He presses his lips into a flat line, and his brows furrow so deeply his dark eyes all but disappear.
* * *
I ask myself if I’d have been any more interested than you are in hearing about lymphedema before this happened to me, but I honestly can’t guess. I’m not even sure I would have believed it if a fellow cancer veteran had tried to explain her own experience of lymphedema. Did this person misunderstand something her doctor said? I’d wonder. How can this even be important if no one has ever heard of it?Now that it’s me, though, I’m living this strange reality in which the crush injury of a blood pressure cuff will cause further damage to delicate lymph vessels, and injections or lab tests unbalance the careful choreography of lymph flow into and out of my limbs. Repetitive movements are off limits for me now, as is leaning my weight on my arms: no more crocheting or spinning wool, no more yoga downward dog.
* * *
“A golf cart, then,” says Tony, days after our pick-up truck discussion. “I don’t need a driver’s license for that.”“No, I guess not,” I tell him. “But you’d have to play golf.”
He ponders that a long moment. “A bike, then,” he says, and this time he’s peering directly into my face.
We’re bargaining, bringing lofty dreams into synch with our limiting realities—his and mine both. I want to give in and say yes, but his lack of critical judgment makes solo riding a nightmare. “Remember when that car rolled right over you?” Miraculously he wasn’t hurt when a neighbor backed out of his drive, right into Tony’s path. Boy and bike disappeared beneath the chassis—fortunately directly between the wheels. That was years ago but the memory is vivid. His eyes narrow, and he nods.
“A tandem,” I counter then. But as soon as the words leave my mouth I realize I’ve gone too far. When I lean my weight on those handlebars my arms will swell despite the hours a day I spend tending my traitorous lymph system.
“Okay,” he says, surrendering. “A tandem.” He flashes me a shy smile.
Suddenly nothing else matters—not the lymphedema, not even the autism. We’re going to make this work, Tony and me. We’ll figure out how to raise the handlebars and keep the weight off my arms. I’ll do the steering, but it will be Tony behind me, providing the pedal power, feeling the bracing whoosh of wind as we race along.
Maybe it’s not a garbage truck, but if the neighbors never line up along the sidewalk to cheer as we ride by, they’ll be missing a beautiful thing.
If you'd like more information about breast cancer-related lymphedema, for yourself, a friend or a family member, please visit stepup-speakout.org
Monday, October 22, 2012
Monday, October 15, 2012
Lymphedema's Emotional Challenges
Lymphedema's Emotional Challenges
http://journals.lww.com/oncology-times/blog/onlinefirst/pages/post.aspx?PostID=541
http://journals.lww.com/oncology-times/blog/onlinefirst/pages/post.aspx?PostID=541
Wednesday, October 3, 2012
Tuesday, October 2, 2012
Dear friends and colleagues,
I am excited to share with you that the new Fix-It and Forget-It PINK Cookbook, a special edition of The New York Times bestselling cookbook, will help benefit the Avon Foundation Breast Cancer Crusade. This special edition features 700 great slow-cooker recipes with a 64-page bonus section featuring inspiring breast cancer survivor stories, their recipes, breast health information and tips.
For every copy of PINK sold the publishers will donate a minimum of one dollar to the Avon Foundation Breast Cancer Crusade. The momentum generated by hitting the bestseller list (largely based on sales during the first week in October) will spur additional sales and more money for the fight against breast cancer.
Please consider purchasing this cookbook for yourself and as a gift for a friend. Share this with your friends and family and be sure to post on your Facebook and other social media outlets.
http://fix-itandforget-it.com/
I am certain you will enjoy every Fix It and Forget It recipe.
Regards,
Marc
Marc Hurlbert, Ph.D.
Executive Director
Avon Foundation for Women Breast Cancer Crusade
I am excited to share with you that the new Fix-It and Forget-It PINK Cookbook, a special edition of The New York Times bestselling cookbook, will help benefit the Avon Foundation Breast Cancer Crusade. This special edition features 700 great slow-cooker recipes with a 64-page bonus section featuring inspiring breast cancer survivor stories, their recipes, breast health information and tips.
For every copy of PINK sold the publishers will donate a minimum of one dollar to the Avon Foundation Breast Cancer Crusade. The momentum generated by hitting the bestseller list (largely based on sales during the first week in October) will spur additional sales and more money for the fight against breast cancer.
Please consider purchasing this cookbook for yourself and as a gift for a friend. Share this with your friends and family and be sure to post on your Facebook and other social media outlets.
http://fix-itandforget-it.com/
I am certain you will enjoy every Fix It and Forget It recipe.
Regards,
Marc
Marc Hurlbert, Ph.D.
Executive Director
Avon Foundation for Women Breast Cancer Crusade
Wednesday, September 26, 2012
ONS PEP Symptom Management Lymphedema App
Publisher's Description
From KiwiTech: Discover evidence-based interventions for Lymphedema, a common side effect of cancer and its treatment. This app is produced by the Oncology Nursing Society (ONS), a professional organization of more than 36,000 cancer nurses and other healthcare professionals. You can find more ONS resources at www.ons.org and www.TheCancerJourney.org.
Read more: ONS PEP Symptom Management - Lymphedema - CNET Download.com http://download.cnet.com/ONS-PEP-Symptom-Management-Lymphedema/3000-2129_4-75232070.html#ixzz27bPZ9IxF
LymphTracker App Now Available in App Store
LymphTracker
An app to manage lymphedema so that you can get back to your life. Send detailed measurement reports to your doctor ...lymphtracker.com/iPhone, iPad, and iPod Touch
LymphTracker is a universal app on the App Store. Maximize the effectiveness of your treatment by trying both the mobile and tablet versions.
American Lymphedema Framework iPhone/iPad App to find LE Therapists
Look4LE
Look4LE is an app brought to you by the American Lymphedema Framework Project (ALFP). In addition to providing links to a variety of resources about lymphedema, the app allows users to search by name or geographic location (using their current location, city or zip code) to identify specialists in their area. Each therapist can provide his or her contact information, including phone number, email address, and website to be displayed on a personal profile page. Additionally, users can get directions to the specialist or even add the information to the system address book. Currently there are over 900 therapists in the directory, and the list will continue to grow as more specialists opt-in.
How It Works
The American Lymphedema Framework Project (ALFP) maintains a list of therapists across the country. The list is updated and made available from the app in both a directory and a map view.
American Lymphedema Framework iPhone/iPad App to find LE Therapists
Go to the Apple App Store on your device. Search for Look4LE
Download app and find a therapist
How to Monitor Your Arm for Lymphedema after Breast Cancer
How to Monitor Your Arm for Lymphedema after Breast Cancer
Tuesday, September 25, 2012
Breathinig
I had a conversation with a masseuse yesterday. He mentioned how most of his clients have compromised lymphatic movement, and the first thing he teaches them is therapeutic breathing. So I asked him about breathing, specifically. We know about breathing in through the nose, out through the mouth, getting a good tummy breath, right? What he added was the importance of a full abdominal tightening/crunch which includes the butt and a kegel squeeze at the end of the exhale. Then the inhale is started by abdominal relaxation, then filling the lungs. I found it to be helpful. - kcshreve
Tips for keeping Cuticles and Fingers Moisturized and Crack-Free
kcshreve
shares her cuticle/finger moisturizing suggestions:
I thought there would be others who may want to share their "tricks" as to how to prevent dryness/cracked skin in fingers which are regularly being wrapped. I have dry skin to begin with, so this has been an increasing problem. I've had good success this week (finally) by using an emollient lip moisturizer by Alba instead of the lotion I was trying. Just before wrapping the fingers, I've been putting this on the cuticles. They've been looking better every morning and today, for the first time in forever, I have no hangnails. Yay! What else has worked for y'all? (I can say that while I'm still living in TX.)
jinky shares her cuticle/finger moisturizing
suggestions:
Any other helpful suggetions?
For me Bag Balm is the only thing that works for me.....put some in thin gloves at night and those oh so sore cracked splits near the nail get fixed up. Also can put it on during the day but the smell isn't good but I don't care as it works. This is what the farmers use on the cows teats. It works........le hugs jinky .....antiseptic to and cost $15 in Canada.
History of Lymphedema
About the only good thing you can say about lymphedema is that its international symbol is the butterfly. Graceful, colorful, ephemeral! It's an emblem we all wish we could emulate as we lumber through the day with our unwieldy wrapped arm or our awkward gloves.
So we've been searching for the history of this symbol and, while we've uncovered some interesting theories, we still don't know whom to thank for this bright spot in our lymphedema experience. Our search continues, but in the meantime we thought you'd enjoy knowing what we've heard so far.
Ann Erlich over at Lymphnotes tells us that her first lymphedema therapist used the expression "gentle as a butterfly kiss" to describe the soft hand strokes of Manual Lymph Drainage (MLD). Of course if your therapist is also doing massage to deal with those tough areas of scar tissue and fibrosis, that butterfly image might flutter right out the window. But it's still a good reminder for us when we do our own self-MLD to keep our touch light and graceful.
Even more cheering is the meaning behind the butterfly symbolism: exquisite new life emerging from the clumsy and colorless cocoon. Hang in there! Right through the wrapping, the grief and the steep learning curve of therapy, that beauty remains within us, hidden for the moment perhaps, but ready to emerge eventually with all our dreams and passions still intact.
Then again – there are those days. . .
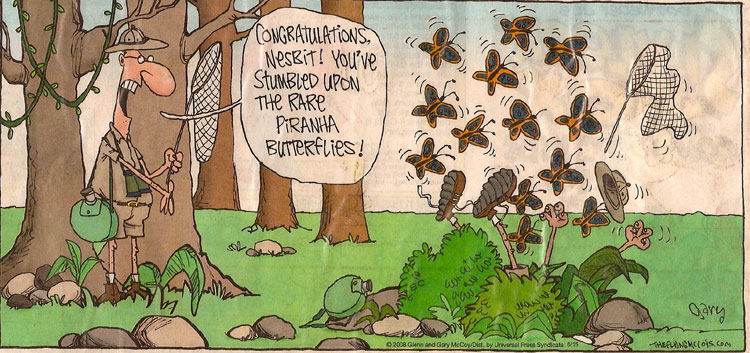
Reprinted by permission of Gary McCoy Copyright 2008
Please visit our page History of Lymphedema to read how this condition existed back in the days of early Egypt, and even affected Royalty.
Monday, September 24, 2012
Series of six Videos of Self MLD by Michigan State University
StepUp SpeakOut shared Lymphedema Guru's status update.
Lymphedema Guru
Great Series of 6 Videos by the Michigan State University on Self-MLD for the Upper Extremity, Home Exercise Program for the Upper and Lower Extremities, and Compression Bandaging for the Arm and the Leg.
Monday, September 17, 2012
Options of Care of Compression Garments
As per Joachim Zuther, on July 29th, 2011 http://www.lymphedemablog.com/2011/07/29/options-of-care-for-compression-garments/
Fabulous One-Handed Cutting Tool
Whether it is due to RIBP or trouble while wrapped, we have been told about a fabulous one-handed cutting tool, making it easy to cut with one hand, whether in food preparation or cutting the food on your plate.
Available at http://www.ulu.com/
Sunday, September 16, 2012
Sunday, September 9, 2012
Monday, August 20, 2012
Saturday, August 18, 2012
Friday, August 17, 2012
Thursday, August 16, 2012
Wednesday, August 15, 2012
Tuesday, August 14, 2012
Manual Lymphatic Drainage: Immune Booster?
About Lindsay Link to original blog posting
In addition to her role as Clinic Director at Toronto Physiotherapy, Lindsay Davey is a Registered Physiotherapist with various post-graduate certifications including Combined Decongestive Therapy, Manual Therapy, and Acupuncture. Prior to completing her Physiotherapy degree Lindsay earned a Master's in Cancer Research at Princess Margaret Hospital in Toronto.
Lymphedema is a form of chronic swelling that occurs in localized areas of the body (such as in a limb) due to impaired lymphatic system function. The lymphatic system normally acts to transport excess fluid back to the heart for redistribution. Congenital lymphatic deficiency or lymph node damage / removal during cancer therapy can disrupt this system, resulting in local fluid stagnation and the characteristic swelling. Since white blood cells rely on proper fluid circulation for transportation, it is not surprising that lymphedema-affected limbs exhibit weak immune response, altered transportation of white blood cells, and increased risk of both local infection and cancer. But can this depressed immune activity be recovered through decongestive therapy, a treatment that reduces lymphatic swelling but does not repair the underlying lymphatic system damage? A small pilot study published this past month (Szolnoky, G. et al. J Eur Acad Dermatol Venereol. 2012 Jul 23) examined this very question:
The authors took eight patients with breast cancer-related lymphedema and exposed a small area of their normal and lymphedematous arms to a protein derived from the tuberculosis bacterium. They measured the resulting immune response and found, as expected, that it was suppressed in lymphedematous arms relative to healthy arms. Next, they treated patients with manual lymphatic drainage and compression therapy over a two week period and re-tested immune response. Patients receiving therapy not only experienced a significant reduction in limb size, but also a substantial boost in immune response – and in only two weeks.
This study and the related body of research suggest something very poignant to individuals suffering from chronic swelling: not only is there a direct negative relationship between swelling and immune function, immune activity can be boosted almost immediately through effective management practices such as manual lymphatic drainage massage and compression.
Monday, August 13, 2012
Attai: A vital question for all women: Are you dense?
By the time I see my breast cancer patients, many of them already know their diagnosis. All are shaken by the discovery of cancer, especially those whose cancer was found belatedly and who thought they had done everything right — regular mammograms and self-exams — to catch any cancer early.
While tumor biology often dictates the course and aggressiveness of the disease, early detection can improve the chances of survival, which is why doctors recommend regular mammograms.
Yet, as a surgeon specializing in the treatment of breast disease, I know that mammography is far from ideal. This is particularly true for women with a normal and common condition called dense breast tissue — a relatively higher concentration of glandular tissue to fatty tissue.
But while normal and common, the added risk presented by dense breast tissue is not well known among women, which is why the California Legislature declared last Wednesday "Are You Dense? Day," as was called for in a resolution authored by state Sen. Joe Simitian, D-Palo Alto.
The goal of "Are You Dense? Day" was to inform women that dense breast tissue both increases the risk of cancer and makes it harder to detect. Dense breast tissue is present in approximately 40 percent of all women undergoing mammograms. Yet, fewer than 10 percent of women are aware of their breast density.
Women who are aware of their breast density, and who talk to their physicians about it, are more likely to discover any abnormalities early in their development. Every year in this country, approximately 200,000 women will be diagnosed with breast cancer, and approximately 40,000 will die from it. A woman with dense breast tissue is four to five times more likely to develop cancer than a woman without it.
The breast is a very difficult and complex organ to image. Because both dense breast tissue and cancer and calcifications create a mammogram image that is mostly "white," looking for cancer amid dense breast tissue has been described as "trying to find a polar bear in a snowstorm."
A woman with dense breast tissue has a 50 percent to 75 percent chance that her cancer will be missed on a screening mammogram, increasing the likelihood that it will not be detected until a later stage, possibly when it is no longer potentially curable.
In many areas of medicine, patients are given a copy of test results and can ask about results they do not understand. This often does not happen with a mammogram. The federal Mammography Quality Standards Act dictates that centers that perform mammography provide a woman with a "layperson letter," which in very basic terms notes whether an abnormality is present or not. It might commonly say "your mammogram shows no evidence of cancer," along with a recommendation to return in one year.
The patient's physician receives a very different report. It will describe detailed findings, including a notation of the density of the breast tissue such as "due to the breast density, the sensitivity of mammography is limited." Many physicians inform the patient only that the mammogram was "normal." Most women with dense breast tissue do not know that their mammogram might have missed something.
To assure that women receive this information, Senate Bill 1538, introduced by Simitian, would require that the patient's mammogram report include breast density information and suggest further discussion with her doctor of the possible benefits of additional screening.
The root of the word "doctor" is from the Latin docere — "to teach." Physicians should welcome the opportunity to provide patients with information and guidance.
"Are You Dense? Day" seeks to educate women about the importance of asking about their breast density.
If they learn they have dense breast tissue, this should prompt further discussion regarding risk factors and whether additional imaging such as ultrasound or MRI might be helpful, depending on the individual situation. Even though no imaging technique is perfect, supplemental screening increases the chances of discovering cancer, and newer, more sensitive tests are continually being developed.
Only when patients are provided with full test results, placed in proper context, can they partner with their physicians to make decisions that are in their best long-term health interest. Ask your physician, "Am I dense?"
Deanna Attai, M.D., is a breast surgeon at the Center for Breast Care Inc. in Burbank. She has been in practice for 17 years and has focused exclusively on the care of patients with diseases of the breast since 2004.
Read more: http://www.vcstar.com/news/2012/aug/11/attai-a-vital-question-for-all-women-are-you/#ixzz23S5ft2Mj
- vcstar.com
Subscribe to:
Posts (Atom)
Blog Archive
-
▼
2012
(34)
-
►
September
(15)
- ONS PEP Symptom Management Lymphedema App
- LymphTracker App Now Available in App Store
- American Lymphedema Framework iPhone/iPad App to ...
- How to Monitor Your Arm for Lymphedema after Breas...
- Breathinig
- Tips for keeping Cuticles and Fingers Moisturized ...
- History of Lymphedema
- Series of six Videos of Self MLD by Michigan State...
- Lymphedema and Axillary Cording
- Options of Care of Compression Garments
- Lymphedema- New and Emerging Treatments (Part 1)
- Fabulous One-Handed Cutting Tool
- 2012 Fall Newsletter is Out
- Happy New Year!
- The Risk of Breast Cancer Related Lymphedema Over ...
-
►
August
(10)
- Lymphatic Decongestive Exercises for the Arms from...
- Bridging the knowledge gap in hospitals and commun...
- Risk Reductions for Lymphedema
- Complications from breast cancer treatment should ...
- Lymphatic Reconstructive Surgery for Lymphedema: N...
- Avoiding the Airplane Cold | IndependentTraveler.com
- Can Breast Reconstruction Post-Mastectomy DECREASE...
- Manual Lymphatic Drainage: Immune Booster?
- Attai: A vital question for all women: Are you dense?
-
►
September
(15)